Obesity is a complex, chronic, and relapsing non-communicable disease characterised by the abnormal or excessive accumulation of body fat, posing significant health risks. It is recognised as a precursor to numerous other non-communicable and communicable diseases.
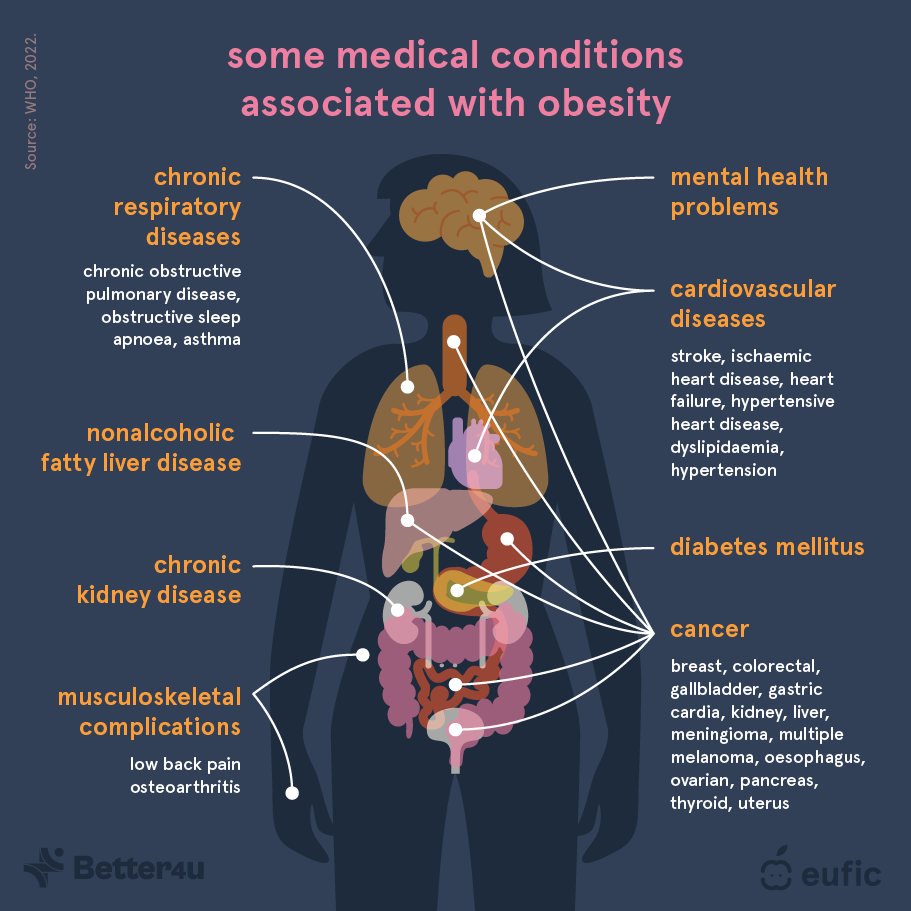
Fig. 1 – Medical conditions associated with obesity;
Better4U partner, The European Food Information Council has written an article on “Obesity: definition, causes and prevention strategies” exploring the underlying causes of obesity and examines strategies for its prevention. Addressing the factors causing obesity through balanced nutrition, regular physical activity, and societal interventions is crucial to reduce the health and economic impacts of obesity. It is essential to recognise that no single solution can reverse the obesity epidemic, and a collaborative, multisectoral approach is required.
📢 Read the full article on EUFIC’s website here.

Fig. 2 – Tips to prevent overweight and obesity throughout the life course.
